Why Definitions Matter – From Labels to Treatment
Words shape reality. And when it comes to gender, they also shape policies, prescriptions, and permanent medical outcomes.
- “Transgender.”
- “Non-binary.”
- “Dysphoria.”
- “Assigned female at birth.”
- “Gender fluid.”
- “Affirmation.”
Why Definitions Matter – From Labels to Treatment
Words shape reality. And when it comes to gender, they also shape policies, prescriptions, and permanent medical outcomes.
- “Transgender.”
- “Non-binary.”
- “Dysphoria.”
- “Assigned female at birth.”
- “Gender fluid.”
- “Affirmation.”
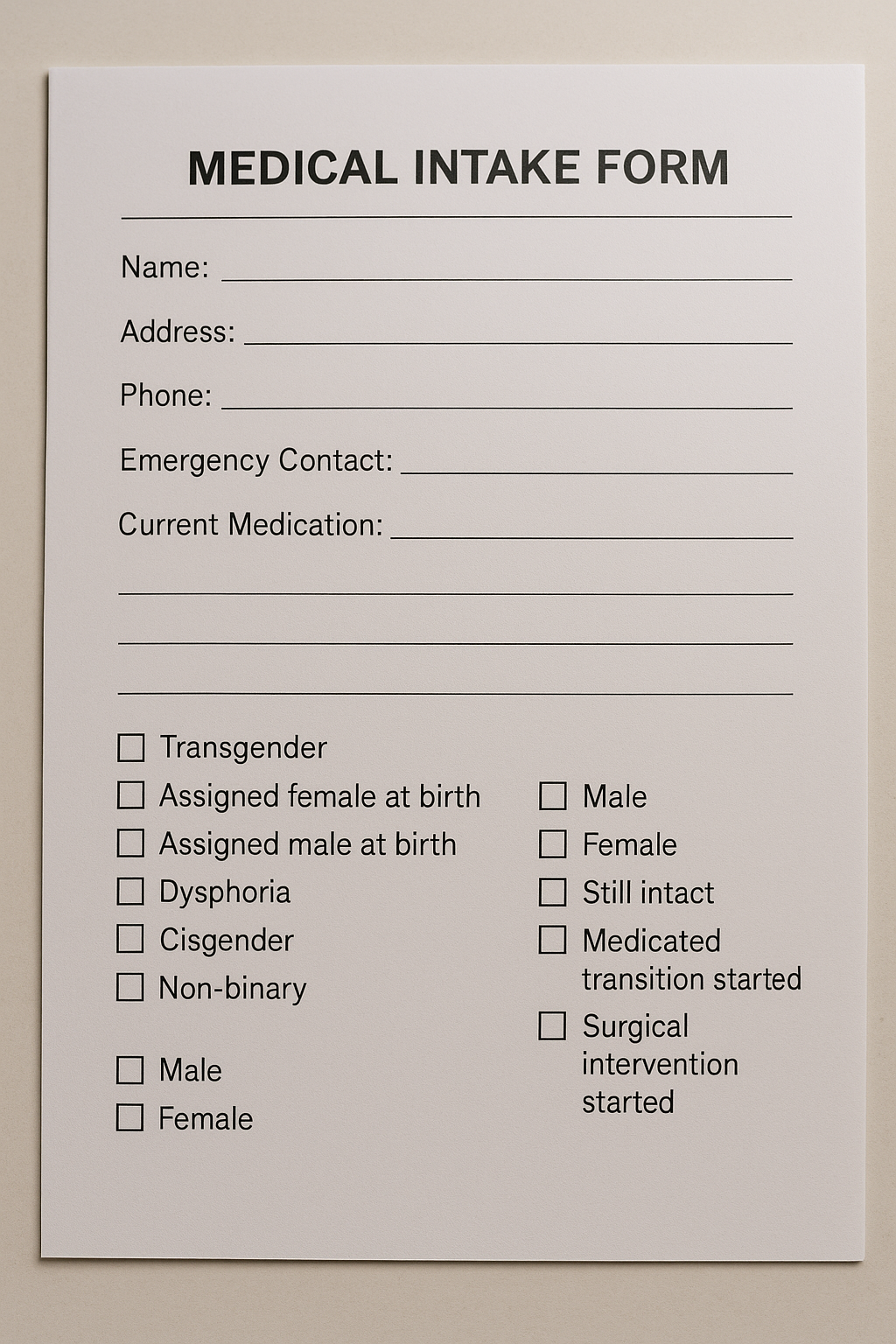
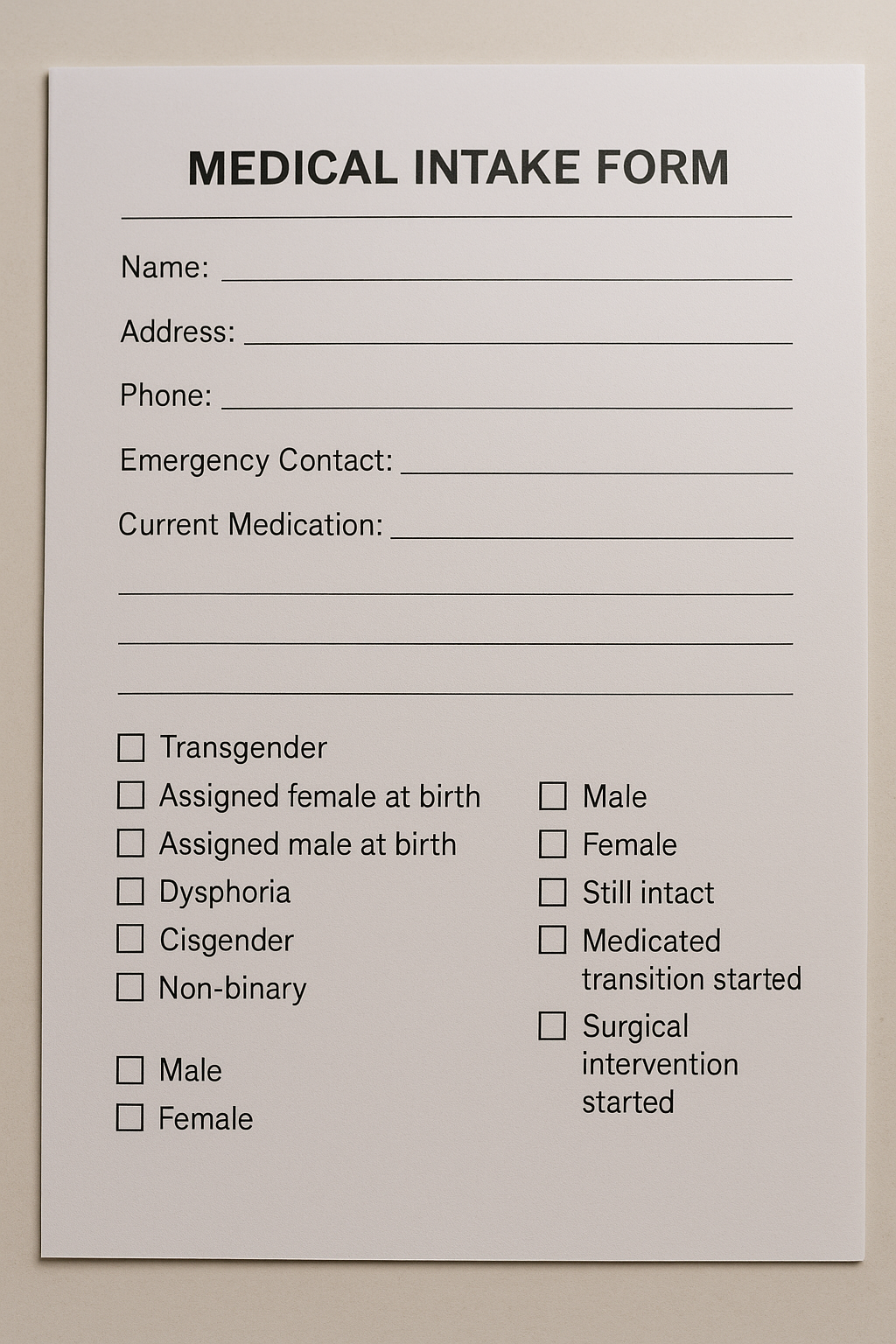
These words aren’t just personal, they’re clinical. They’re used in medical intake forms, insurance codes, research studies, and legal frameworks. And if we get the definitions wrong, we risk getting the treatment wrong too.
Language evolves, and in personal identity, that flexibility can be empowering. But in clinical care, precision has to come first.
From Identity to Action
A label doesn’t stay just a label. In today’s system, a label is often a trigger for action.
- Say “transgender,” and you may be offered hormones.
- Say “gender dysphoria,” and you might qualify for surgery.
- Say “non-binary,” and you could be prescribed the same permanent medications, without a clear diagnostic framework behind it.
This isn’t about language policing. It’s about medical precision.
If we don’t define what we’re treating, how do we know we’re treating the right thing?
The Blurred Line Between Identity and Condition
The line between personal identity and medical condition used to be clearer.
Now? Not so much.
Gender dysphoria is a diagnosis.
Transgender is an identity.
But when identity alone leads to clinical action, the distinction becomes meaningless.
That’s not clarity. That’s chaos.
If we treated diabetes or depression the same way, based solely on someone’s self-applied label, we’d call it malpractice.
So why should gender be treated differently?
Definitions Drive Policy
Insurance doesn’t reimburse for feelings—it reimburses for diagnoses.
Legislation is written based on categories and classifications. Research funding is allocated based on diagnostic codes. Medical boards create treatment guidelines based on what those terms are supposed to mean.
If a term like “gender incongruence” becomes too vague, or “affirmation” gets used to mean everything from clothing to surgery, we lose the ability to track outcomes, study long-term effects, or even agree on what treatment is.
In one clinic, “gender incongruence” might mean distress requiring intervention. In another, it might mean identity discomfort with no clinical impairment.
Two different meanings, same label.
The words we choose shape the world we build. And right now, the foundations are cracking.
The Middle Ground: Define With Care
Respecting a patient’s autonomy is essential—but autonomy isn’t about bypassing evaluation. It’s about being empowered with clarity, not guided by confusion.
This isn’t about restricting how people describe themselves. It’s about making sure the clinical system uses definitions that are clear, testable, and evidence-based, so we don’t make permanent decisions based on shifting meanings.
We don’t need fewer identities.
We need smarter systems that separate self-expression from medical intervention.
Because when the terms are fuzzy, the outcomes are too.
And people deserve more than guesswork.
Your Turn
Do you think our current definitions around gender identity and dysphoria are helping—or confusing—the system?
Sources & Citations
- World Health Organization. (2019). ICD-11: Classifying Gender Incongruence. Link
- Dahlen, S., et al. (2022). Medicalizing Identity: The Role of Language in Gender Dysphoria Diagnosis. Journal of Medical Ethics. Link
- Olson-Kennedy, J., et al. (2016). Mental Health of Transgender Children Who Are Supported in Their Identities. Pediatrics, 137(3). Link
- Levine, S. B. (2021). Reflections on the Clinician’s Role with Individuals Who Self-Identify as Transgender. Archives of Sexual Behavior, 50, 3527–3533. Link